The Ministry of Health has announced a new structured framework to facilitate specialised treatment abroad for Kenyans under the Social Health Insurance (SHI) scheme.
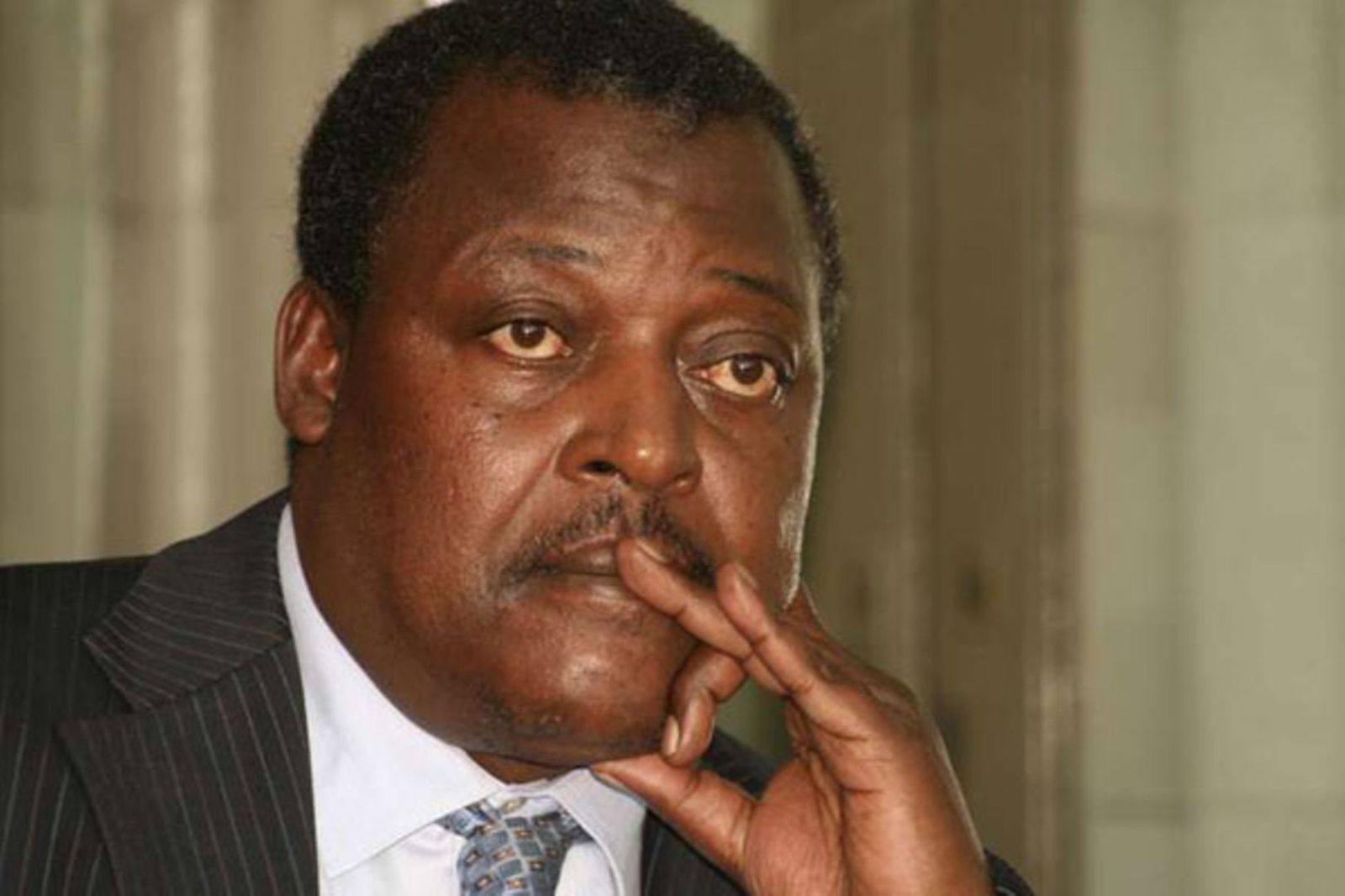
Health Cabinet Secretary Aden Duale said the initiative, implemented through the Social Health Authority (SHA), seeks to ensure no Kenyan is denied access to life-saving medical and surgical procedures that are not available locally.
“This milestone is a testament to the government’s commitment to ensuring that no Kenyan is denied access to life-saving, specialised medical and surgical procedures not yet available locally, while simultaneously strengthening our national health system,” Duale stated in a press release.
The move follows recommendations by the Benefits Package and Tariffs Advisory Panel (BPTAP), which identified 36 medical services unavailable in Kenya.
The list has already been gazetted, and further additions will be made based on continuous health technology assessments.
"This is a preliminary list, as the process of identifying additional interventions is continuous and will be guided by a comprehensive Health Technology Assessment (HTA)," Duale said.
According to the new framework, only overseas health facilities accredited in their home countries and recognised by Kenyan regulators will qualify.
These facilities must also be linked to contracted hospitals in Kenya to guarantee follow-up care once patients return.
"A beneficiary can only access treatment outside Kenya if the healthcare service is not available locally," the CS said.
Further, the beneficiary's contributions must also be up-to-date.
Access to overseas treatment will be limited to SHI beneficiaries whose contributions are up to date and only if the required service is unavailable locally.
Referrals will undergo peer review by the Claims Management Office to verify medical necessity and compliance with the financial limits of the benefits package.
The ministry capped the maximum payable amount for overseas treatment at Sh500,000, subject to revision after contracting and rate negotiations with approved facilities abroad.
Treatments considered unproven, experimental or unconventional will not be covered.
Duale said the SHA Board has been directed to fast-track the empanelment and contracting of foreign hospitals and publish the official list for public access.
“This new framework guarantees a transparent, evidence-based, and accountable system for Kenyans seeking treatment abroad, ensuring value for money and quality care,” the CS added.
The government emphasised that the reform marks a shift from the former NHIF model by embedding stricter legal, financial, and medical guidelines under the Social Health Insurance Act, 2023.