
ARTI SHAH: She has lived with endometriosis for the last 30 years. Photo/ Elisha Singira.
“I started experiencing symptoms as a teenager when my periods began at 13 – excruciating cramps, nausea, fatigue, depression, mood swings, and pain that radiated beyond my pelvic area. As time went on, it escalated to chronic pain, severe digestive issues, and an overwhelming exhaustion that made even simple tasks feel impossible. Studying became incredibly difficult, as I couldn’t focus. For the longest time, I battled depression without realising there was a silent demon within me—culminating in the name of endometriosis,” she explained.
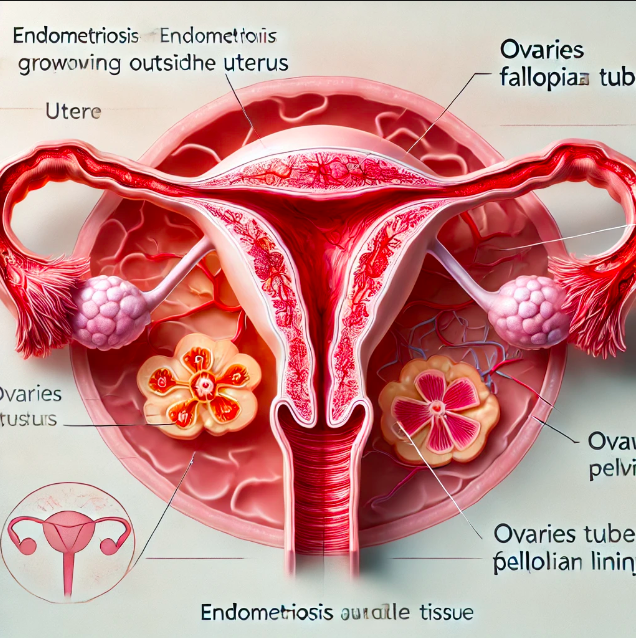
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus. This can cause pain, heavy periods, and sometimes fertility problems. The tissue behaves like normal uterine lining: It thickens, breaks down, and bleeds during each menstrual cycle, but because it has no way to exit the body, it can lead to inflammation, scarring, and pain.
It commonly affects the ovaries, fallopian tubes, and the tissue lining the pelvis. Treatments include pain management, hormone therapy, and sometimes surgery.
Arti continues, “It took me 12 years. I saw countless doctors who dismissed my pain or misdiagnosed it as irritable bowel syndrome, stress, or just ‘bad periods.’ I was placed on various birth control treatments to suppress estrogen production and manage symptoms, both in Kenya and abroad. I had to fight for answers, endure invasive tests, and advocate for myself until I finally got the correct diagnosis. It was both a relief and a heartbreak because I realised how much unnecessary suffering I had endured.”
She says the condition has impacted every part of her life.
Some days, the pain is so intense that she cannot get out of bed.
“I have undergone multiple surgeries. The experience was both hopeful and terrifying. While it provided relief, it wasn’t a cure. Recovery was difficult, but it gave me clarity about my condition and the strength to keep fighting for better care. I underwent multiple ablation surgeries, where adhesions were burned off rather than removed, leading to a higher recurrence rate. Two and a half years ago, I finally had excision surgery abroad, where a trained excision specialist removed the disease at its root. However, six months later, I felt like I was back to battling this same familiar journey, with the same excruciating pain and flare-ups. I was then diagnosed with adenomyosis, the sister condition of endometriosis.”
In December 2024, Arti underwent a major surgery in Kenya for adenomyosis, where doctors found endometriosis had recurred, covering the ureter, intestines, ovaries, and even causing organ fusion.
She says: “Now, I am on the road to recovery, reclaiming my life as much as I can, though I still battle severe IBS and neuropathy. Finding the right specialist made all the difference, but I had to push through so many dismissive encounters to get there.”
Dr Yamal Patel is a consultant obstetrician and gynecologist with special interest in endometriosis and adenomyosis care, works with 3rd Park Hospital.
He explains endometriosis can make it harder to get pregnant. It can start at a person’s first menstrual period and last until menopause.
He says, “It is a benign disease, but it behaves quite radical, almost like cancer because it starts growing into surrounding structures making it chronic. It is something that affects the quality of life of the victims because it affects both physical and psychosocial state of the woman and also affects fertility. It causes fibrosis in very hard nodules and it impacts the surrounding structures.”
He says the diagnosis of endometriosis has been a very complex area to handle so far.
And the reason is until now, worldwide, roughly one in ten women have it. “So, if we just take a population of Kenya with a population of let's say 60 plus million people, and I would believe we would be right in saying there might be around 20 plus million women and girls in the reproductive age group above the puberty age, I would say that imagine 2 million plus women in Kenya have this condition,” he said.
According to the World Health Organization, Endometriosis affects roughly 10 per cent (190 million) of reproductive age women and girls globally. That is between the ages of 15 – 44.
Yamal says the diagnosis is difficult and that the average time of diagnosis of endometriosis from its initial presentation to a doctor to a diagnosis, name of endometriosis, average worldwide has been 7 to 10 years.
He says you have to be careful in listening to the patient to get the information you want.
“They always tell you what they feel and you have to be having a keen ear to the story of these women and girls and it will tell you there's something wrong. Don't dismiss or normalise their symptoms. As a gynecologists examine the patient to understand the problem,” he explains.
“Finally, the mainstay of diagnosis now is ultrasound and imaging. Ultrasound, MRI are very accurate ways in the right trained hands to diagnose endometriosis. Our strive is to reduce this interval from 7 to 10 years to probably even a year or two so that we pick them up early and start managing them.”
With regards to the management of endometriosis, Dr Yamal says, “it's a very complex area, but it should be usually goal-based, preference-based, and then it can be either, medical or surgical or expectant. It has different ways depending on the goal. We base our treatment on the goal and the patient guides us on her needs. Now, we have medical treatments which is mainly suppressive. It's not curative.”
He says there is also complementary and alternative medicine. He says people have tried acupuncture, meditation or yoga or exercise. Some have lifestyle changes with dietary changes or medications like gluten-free or reduced gluten, reduced dairy, reduced red meat, increased cumin.
Other management options are dietary, lifestyle, complementary treatment, medical treatment, surgical treatment, expectorant treatment.
Dr Yamal admits there are a number of misconceptions surrounding endometriosis. He says, “The first is that pain is normal. Pain is never normal. Pain is a body response to a noxious stimulus, which is usually something your body does not want. Number two is that pregnancy is a cure for endometriosis, pregnancy is never a cure for endometriosis because you may or may not get pregnant because of endometriosis. The third thing is endometriosis is like a death sentence. No. When someone is told endometriosis, they feel bad, they start getting worried, upset, depressed. On the contrary, endometriosis is very manageable.”
He says every woman, with or without endometriosis, should be able to get pregnant if the condition is picked correctly, early and managed early. Some may need treatment, medication, some procedures, some may need artificial reproductive technology, including IVF, but getting pregnant is possible. “So not being possible to get pregnant is not an option and finally people should understand that endometriosis is not cancer.”
Arti Shah says there is a lot that people need to know in regards to endometriosis. “People should know that it is not ‘just a bad period.’ It is not a reproductive condition—it has been found in every part of the body. It’s unpredictable, exhausting, and can be disabling. It’s a very isolating condition, which is why emotional support and being heard are crucial. Awareness must shift beyond just period pain to the full complexities of the disease.”
She advises people with the condition: “You are not
alone and your pain is real. Keep fighting for answers, find a supportive
community, and never let anyone dismiss what you’re going through. You deserve
care, understanding, and relief. Be your own advocate, take the time to
understand your body, your symptoms, and your triggers.”
After her experience, advocacy has become her purpose. She now works to educate and support others while pushing for better healthcare.
“I work with Endo Sisters East Africa to provide support for those navigating this journey. I also collaborate with Yellow Endo Flower on advocacy initiatives. We fight so the next generation doesn’t have to endure what we have. No one should have to navigate this alone. I am calling on the government to enhance early diagnosis for the patients in all areas.”
Arti says education about endometriosis needs to start early—in schools, workplaces, and other organisations. If young people, teachers, employers, and the medical community are informed, we can break the cycle of misdiagnosis and delay. Doctors need more specialized training, and awareness must move beyond just reproductive health discussions. Endometriosis affects every part of the body, and its impact needs to be recognized at every level of society.












